The implementation of knowledge translation frameworks into policy is imperative for addressing the discrepancy between research and decision-making. Despite substantial progress in evidence generation, numerous research findings fail to influence policy due to barriers such as misalignment of research priorities, inadequate communication between researchers and policymakers, and the intricacy of policy processes. Various frameworks have been developed to enhance the integration of research into policy, emphasizing factors such as acceptability, feasibility, scalability, and sustainability. These frameworks aspire to guarantee that research findings are not only generated but also effectively implemented to enhance healthcare outcomes and public health strategies.
The SPIRIT Action Framework →
The SPIRIT (Supporting Policy In health with Research: an Intervention Trial) Action Framework was designed to enhance the integration of research into policy by providing a structured method for selecting and evaluating strategies that support research use. The framework was developed in response to the proliferation of knowledge translation strategies, which, despite their increasing prevalence, often lack systematic organization and empirical validation.
Implementability of Healthcare Interventions →
The paper explores the concept of implementability, defined as the likelihood that a healthcare intervention will be successfully adopted and sustained in real-world settings. Despite a growing body of research on implementation science, many interventions fail to achieve long-term uptake due to a lack of planning for scalability and sustainability.
Research for Policy tool →
Effective knowledge utilization in policy making requires proper alignment between researchers and policymakers. This tool serves as a checklist for both researchers and policymakers, helping them address key alignment areas throughout a research project. Maintaining alignment between these two groups during the research process can be challenging, making this tool particularly valuable for all researchers seeking to align their work with policy needs.
Knowledge to Action →
The Knowledge to Action (K2A) Framework outlines three phases - research, translation, and institutionalization and the decision points, interactions, and support structures within the phases that are necessary to move knowledge into sustainable action. It is designed for facilitators, practitioners and researchers, providing a structured approach to bridging research and practice, and control of chronic diseases.
Lost in Knowledge Translation →
This article addresses the challenge of translating research findings into real-world healthcare practice. It highlights the confusion surrounding terms like knowledge translation, transfer, and exchange, and proposes a conceptual framework to clarify the process of moving knowledge into action.
Model for Value-Based Policy-Making in Health Systems →
This article examines the role of values in health policy-making. It argues that while values are central to discussions about health systems and their reform, the concept of "value" itself remains vague, and policy-making processes often neglect values. The study aims to provide a model for value-based policy-making to clarify the concept of value and how it affects policy decisions.
JBI's Approach to Evidence Implementation →
In the ever-evolving field of healthcare, the seamless integration of evidence into practice remains a persistent challenge. While various theoretical models and frameworks exist to guide implementation efforts, healthcare professionals often grapple with the practicalities of translating research into real-world clinical and policy settings. This paper introduces and describes the JBI's approach to evidence implementation, outlining a pragmatic and structured seven-phase process model designed to bridge the gap between evidence and practice.
Review of Frameworks for Translating Research Evidence into Policy and Practice →
The need to find unified approach for research translation: importance of a common language across disciplines, implementation of frameworks yes, but also monitoring scaling interventions.
The SPIRIT (Supporting Policy In health with Research: an Intervention Trial) Action Framework
Background
The SPIRIT (Supporting Policy In health with Research: an Intervention Trial) Action Framework was designed to enhance the integration of research into policy by providing a structured method for selecting and evaluating strategies that support research use. The framework was developed in response to the proliferation of knowledge translation strategies, which, despite their increasing prevalence, often lack systematic organization and empirical validation.
Framework
The framework suggests a four-step pathway for research use in policy:
- Catalysts for Research Use: A stimulus or external factor, such as a policy crisis, public demand, or an urgent health issue, that prompts policymakers to seek research-based solutions;
- Organizational Capacity: The ability of a policy agency to effectively engage with research, including having skilled personnel, supportive policies, and access to relevant research;
- Engagement Actions: The specific strategies used by policymakers to interact with research, including accessing evidence, appraising its quality, commissioning new research, and collaborating with researchers.
- Research Use: The application of research in policymaking, which can be instrumental (directly informing decisions), conceptual (shaping thinking), or strategic (used to justify actions).
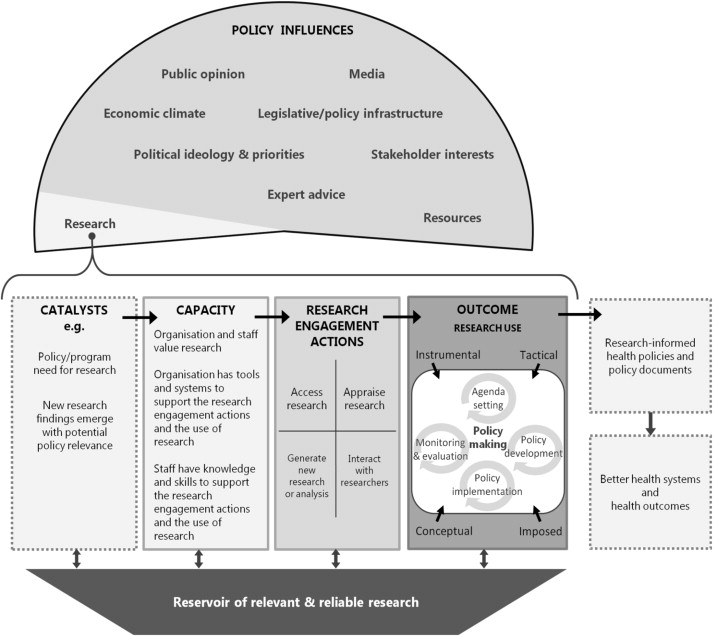
Key insights and implementation considerations
Agencies must understand the drivers behind the use of research and must be able to determine the types of strategies for those agencies.
- Recognize when the appropriate circumstances or timing of the release of research occurs
- Increase agency and staff's value of research by giving explicit acknowledgement
- Increase and improve agencies resources that staff members will use for using research
- Improve staff skills for all stages of the research to action cycle
- Access, Appraisal and Interaction with Researchers
- Engage policy development staff in activities that stimulate innovative or strategic actions.
Conclusion
The SPIRIT Action Framework provides a structured, evidence-informed approach for organizations to guide efforts in linking research with policy-making. This framework emphasizes the importance of tailoring strategies to the unique context and the need to create a reservoir of relevant and reliable research to stimulate research use and improve health outcomes.
Reference
Redman, Sally & Turner, Tari & Davies, Huw & Williamson, Anna & Haynes, Abby & Brennan, Sue & Milat, Andrew & O'Connor, Denise & Blyth, Fiona & Jorm, Louisa & Green, Sally. (2015). The SPIRIT Action Framework: A structured approach to selecting and testing strategies to increase the use of research in policy. Social Science & Medicine. 136-137C. 10.1016/j.socscimed.2015.05.009.
Implementability of Healthcare Interventions
Background
The paper explores the concept of implementability, defined as the likelihood that a healthcare intervention will be successfully adopted and sustained in real-world settings. Despite a growing body of research on implementation science, many interventions fail to achieve long-term uptake due to a lack of planning for scalability and sustainability. This article addresses the need to reduce research waste by focusing on factors that influence the uptake of evidence into practice, including acceptability, fidelity, feasibility, scalability, and sustainability.
Framework
Five core concepts influencing implementation are developed:
- Acceptability: The degree to which an intervention is perceived as suitable and appropriate by stakeholders, including both providers and recipients
- Fidelity: The extent to which an intervention is delivered as intended, ensuring that the core components remain intact
- Feasibility: The practicality of implementing an intervention, considering available resources, workforce capacity, and organizational constraints
- Scalability: The potential for expanding an intervention beyond its initial setting to other populations or regions
- Sustainability: The long-term maintenance of an intervention’s effectiveness within routine practice
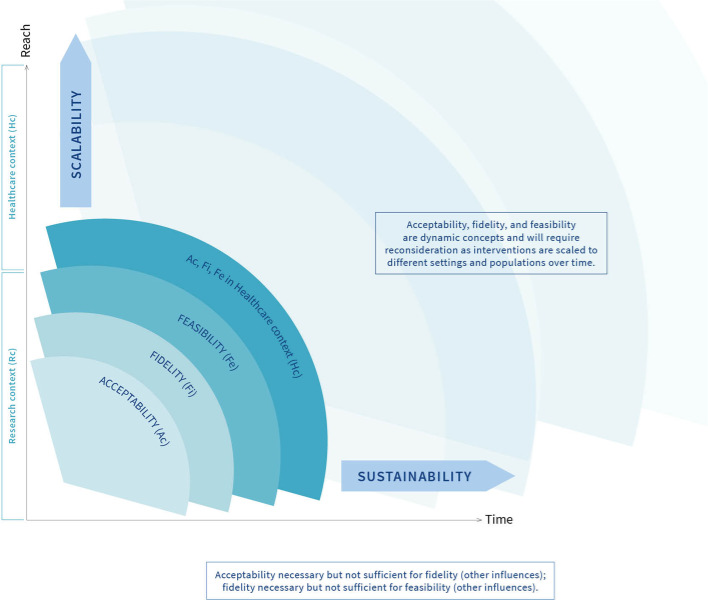
Key insights and implementation considerations
For healthcare interventions to be successfully implemented, researchers need to consider not only their effectiveness but also their "implementability". This includes considering the views and practical concerns of those delivering and receiving the intervention. The implementability framework is proposed as a chronological, iterative approach, emphasizing that these factors should be addressed from the early stages of intervention development, evaluation, and implementation, and revisited over time as interventions scale and adapt.
- During the design and initial evaluation phases: Actively seek input and feedback from stakeholders such as patients, clinicians, or system administrators regarding perceived worth, practicality, and integration ease. Assess all the enablers of acceptability and how the intervention can provide positive outcomes Seek information of the training and supervision and review guidelines
- Scalability with Sustainability: With proven acceptability, feasibility and fidelity the project team should broaden their scope to seek ways to enhance sustainability Conduct research to learn how to facilitate the program among partners Seek how to make cost-effective and ethical
Conclusion
The authors conclude that by proactively and iteratively addressing acceptability, fidelity, and feasibility during the intervention design, evaluation, and implementation phases, researchers can improve the likelihood of scalable and sustainable uptake, ultimately reducing research waste and improving healthcare outcomes.
While the framework must be used for different interventions over time it requires continuous innovation to facilitate long-term success.
Reference
Klaic M, Kapp S, Hudson P, Chapman W, Denehy L, Story D, Francis JJ. Implementability of healthcare interventions: an overview of reviews and development of a conceptual framework. Implement Sci. 2022 Jan 27;17(1):10. doi: 10.1186/s13012-021-01171-7. PMID: 35086538; PMCID: PMC8793098.
Research for Policy tool
Background
This study seeks to address the persistent challenge of misalignment between research production and policymaking. Despite decades of efforts to enhance research uptake, many studies have failed to influence policy due to a lack of structured interaction between researchers and policymakers. To address this gap, the authors developed the Research for Policy (R4P) tool, a structured reflection tool designed to help researchers align their work with policy needs by providing practical guidance and facilitates reflection on process issues in research projects.
Framework
It identifies eight key alignment areas that researchers must consider to improve policy impact:
- Goal alignment: Ensuring that research objectives match policymakers’ needs.
- Research quality: Delivering credible, relevant, and timely findings.
- Relevance & timing: Providing evidence at the right moment in the policymaking cycle.
- Tasks & authority: Clarifying the roles of researchers and policymakers to ensure collaboration and accountability.
- Consultative structure: Establishing effective communication channels between researchers and decision-makers.
- Vertical alignment: Ensuring that research priorities align with both frontline policy needs and higher-level strategic goals.
- Organizational environment: Understanding the broader institutional and political context affecting research use.
- Presentation & accessibility: Delivering findings in formats that are usable for policymakers (e.g., policy briefs instead of lengthy reports).
Download final version of the R4P
Key insights and implementation considerations
For researchers to maximize the impact of their work on policy, they should systematically reflect on key alignment areas throughout the research process. The R4P tool facilitates this reflection through a series of open-ended questions.
- Get acquainted with the eight alignment areas:
- Goal: The clarity of expectations and purpose
- Tasks and Authority: Clear definition of tasks and responsibilities
- Quality: Research method, conceptual framework and data
- Consultative Structure: Effective stakeholder
- Vertical alignment: Understanding and addressing issues
- Organizational Environment: Factors
- Relevance and Timing: Formulation and wording of results; timely delivering
- Presentation: The structure of tools and what strategy to extract knowledge
- A central point of reflection is to focus the questions to be more related to the goal of the project
- Implement the 23 reflection questions and with the help of illustrations, to be familiarized with the aspects (see link above) In all phases of the intervention make an effort to focus on the question
- Use the tool as a basis for open discussion within the project team to improve collaboration
- Review and customize if desired: Integrate to the questions in this process
Conclusion
The R4P tool offers researchers practical guidance for improving alignment with policymakers. By facilitating reflection on process issues and the consideration of context-sensitive factors, the tool supports researchers in acting in ways that are more likely to have a meaningful impact on policy. Ultimately, this framework contributes to the goal of enhancing the contributions of research to evidence-based policymaking.
Reference
Hegger, I., Marks, L.K., Janssen, S.W. et al. Research for Policy (R4P): development of a reflection tool for researchers to improve knowledge utilization. Implementation Sci 11, 133 (2015). https://doi.org/10.1186/s13012-016-0496-1
Knowledge to Action
Background
The Knowledge to Action (K2A) Framework outlines three phases - research, translation, and institutionalization and the decision points, interactions, and support structures within the phases that are necessary to move knowledge into sustainable action. It is designed for facilitators, practioners and researchers, providing a structured approach to bridging research and practice.and control of chronic diseases.
Framework
It explores 3 key components:
- Phases of Translation: The framework identifies three main phases: Research Phase: Involves generating and testing scientific discoveries to assess their relevance for translation. Translation Phase: Focuses on transforming scientific knowledge into actionable tools (e.g., programs, policies) and ensuring their implementation. Institutionalization Phase: Marks the maintenance and integration of interventions into routine public health practices.
- Supporting Structures and Evaluation: All phases require robust supporting systems, such as funding, training, organizational capacity, and leadership, to ensure success. Evaluation plays a critical role throughout to measure impact and refining processes.
- Bidirectional Interaction: Effective translation necessitates collaboration between researchers and practitioners. This includes using practice-based discoveries to inform research and returning evidence-based solutions to the field.
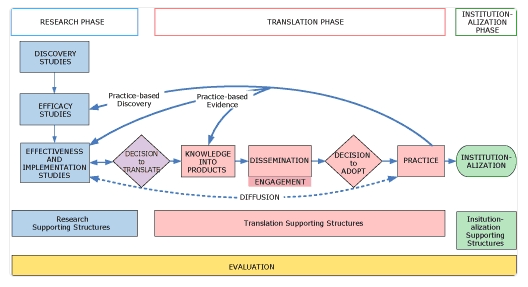
Conclusion
The keys to success in addressing public health challenges, such as the prevention of chronic disease, are meticulous planning, effective stakeholder engagement, and continuous evaluation. The need for collaboration among researchers, practitioners, and policymakers is crucial to achieving meaningful public health outcomes.
Reference
Wilson KM, Brady TJ, Lesesne C; NCCDPHP Work Group on Translation. An organizing framework for translation in public health: the Knowledge to Action Framework. Prev Chronic Dis. 2011 Mar;8(2):A46. Epub 2011 Feb 15. PMID: 21324260; PMCID: PMC3073439.
Lost in Knowledge Translation
Background
This article addresses the challenge of translating research findings into real-world healthcare practice. It highlights the confusion surrounding terms like knowledge translation, transfer, and exchange, and proposes a conceptual framework to clarify the process of moving knowledge into action.
The Knowledge-to-Action (KTA) Framework
The KTA framework consists of two interconnected cycles:
- Knowledge Creation (The Knowledge Funnel)
- Knowledge Inquiry: The broad body of primary research.
- Knowledge Synthesis: Systematic reviews and meta-analyses that aggregate and evaluate evidence.
- Knowledge Products & Tools: Guidelines, decision aids, and frameworks designed to make evidence more accessible and actionable.
- Action Cycle (Application of Knowledge to Practice & Policy)
- Identifying a Problem: Determining an issue that requires an evidence-based solution.
- Adapting Knowledge to the Local Context: Ensuring that evidence is relevant to the specific setting.
- Assessing Barriers to Knowledge Use: Identifying obstacles in the implementation process.
- Selecting & Implementing Strategies: Choosing appropriate interventions for knowledge uptake.
- Monitoring Knowledge Use: Evaluating the application of research in practice.
- Evaluating Outcomes: Assessing the effectiveness of the implemented change.
- Sustaining Knowledge Use: Ensuring long-term integration of research findings into practice.
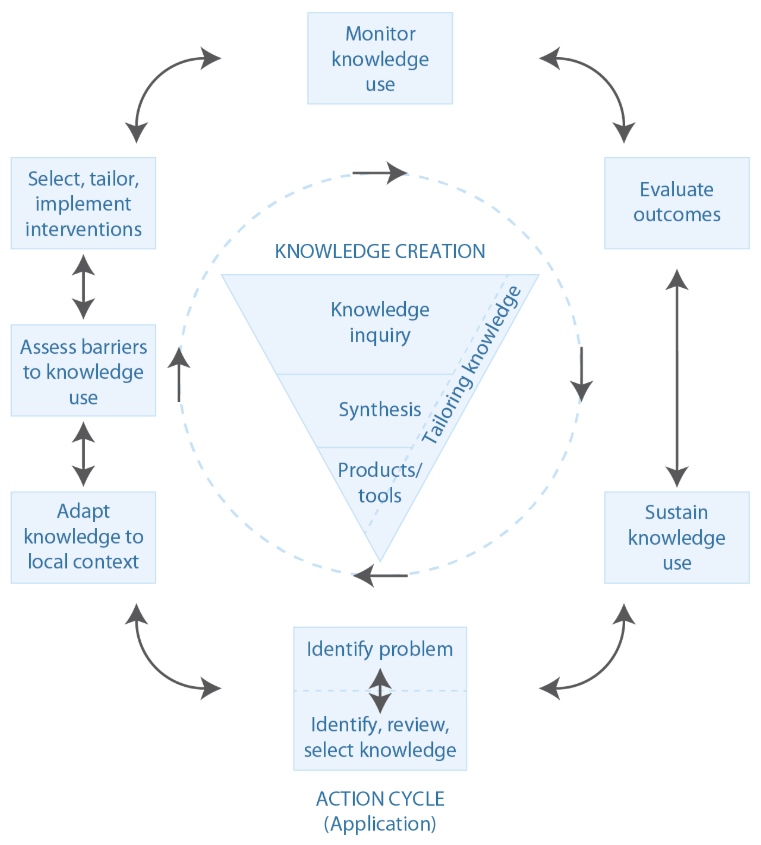
Key insights and implementation considerations
To begin, we have to define our target and what "moving knowledge into action" means. Too often researchers focus on making reports and academic papers. However, there are a plethora of alternative options that facilitate KTA: synopses in ACP Journal Club, care guidelines, decision aids, care pathways, creating better awareness and training for policymakers. This is the start of the planned-action theories and frameworks to help influence change in practice settings. The model suggests that to be effective in the real world, these interventions must be carefully tailored to fit local settings and circumstances. At all levels of planning, the user should consider such important steps as: establishing organizational buy-in, finding support from sources such as marketing, training, and technical assistance. The goal is to create a model to identify the relevant stakeholders and to establish a common understanding of KTA.
Conclusion
The authors conclude that because of a lack of consensus on what moving scientific research into policy is, a variety of processes and stakeholders must be included. In addition, there should be a clear articulation of responsibilities at all levels, as well as support and training from outside experts. The goal is a cycle of improvement that will be repeated and improved by the user.
Reference
Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006 Winter;26(1):13-24. doi: 10.1002/chp.47. PMID: 16557505.
Model for Value-Based Policy-Making in Health Systems
Background
This article examines the role of values in health policy-making. It argues that while values are central to discussions about health systems and their reform, the concept of "value" itself remains vague, and policy-making processes often neglect values. The study aims to provide a model for value-based policy-making to clarify the concept of value and how it affects policy decisions.
Framework: The Value-Based Policy-Making Model
The model consists of four key components:
- Terminal Values:
- The ultimate goals that policies aim to achieve (e.g., health equity, well-being, sustainability).
- These values are shaped by ethical ideologies and influence high-level policy decisions.
- Instrumental Values:
- The means through which terminal values are achieved (e.g., efficiency, affordability, accessibility).
- These values guide the selection of strategies for policy implementation.
- Criteria System:
- Converts abstract values into measurable indicators.
- Helps policymakers assess whether a policy aligns with key values.
- Evidence Integration:
- Ensures that policy decisions are based on scientific evidence, while respecting societal values.
- Acknowledges that different countries prioritize different value frameworks, affecting evidence interpretation.
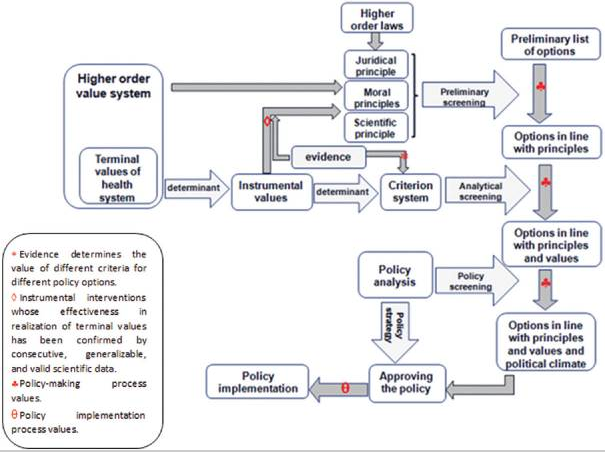
Key insights and implementation considerations
An effective health policy-making should be explicitly based on a clear and consistent understanding of values.
- Defining Terminal Value Framework: Policymakers must first define the relationship of values to each other and their priorities.
- Determining Instrumental Values: As the importance of the terminal values must determine the relation of the instrumental values to the realization of terminal values.
- Establishing a Criteria System: Criteria are selected as less abstract intermediaries between values and decision-making, their relationship and the importance of each other must be determined.
Conclusion
The article concludes that value-based policy-making is essential for effective health system reform. By making values explicit and transparent, policymakers can avoid blindly imitating other experiences and create policies tailored to the unique needs and values of their country. The study's model provides a framework for understanding the complex interplay of values, evidence, and other factors in the policy-making process, ultimately leading to better health outcomes.
Reference
Shams L, Sari AA, Yazdani S, Nasiri T. Model for Value-based Policy-making in Health Systems. Int J Prev Med. 2021 Feb 24;12:13. doi: 10.4103/ijpvm.IJPVM_325_19. PMID: 34084310; PMCID: PMC8106279.
JBI's Approach to Evidence Implementation
Background
In the ever-evolving field of healthcare, the seamless integration of evidence into practice remains a persistent challenge. While various theoretical models and frameworks exist to guide implementation efforts, healthcare professionals often grapple with the practicalities of translating research into real-world clinical and policy settings. This paper introduces and describes the JBI's approach to evidence implementation, outlining a pragmatic and structured seven-phase process model designed to bridge the gap between evidence and practice.
Framework: The JBI Seven-Phase Process Model
A seven-phase process model:
- Identify the Practice Area:
- The process starts with the collaborative identification of a specific practice area or problem requiring improvement, involving key stakeholders such as clinicians, managers, and even patients, to ensure relevance and buy-in.
- Engage Change Agents:
- Engage leaders, facilitators and clinical champions to undertake the initiative.
- Assess Context and Readiness for Change:
- A thorough context analysis is conducted to understand the unique factors influencing the proposed change, examining aspects like organizational structure, workplace culture, communication systems, and resource availability.
- Review Practice Against Evidence-Based Audit Criteria:
- Current practices are then rigorously compared against evidence-based audit criteria to identify areas for improvement, utilizing established guidelines and standards.
- Implement Changes to Practice Using Getting Research into Practice (GRIP):
- Based on the audit findings, barriers and enablers to evidence utilization are identified, and tailored implementation strategies are developed and implemented using the GRIP method.
- Re-Assess Practice:
- Following implementation, practice is reassessed to evaluate the impact of the changes and identify any remaining gaps.
- Plan for Sustainability:
- Finally, sustainability is addressed by embedding the changes within the organizational culture and establishing mechanisms for ongoing monitoring and improvement.
Key insights and implementation considerations
This framework should be implemented with a focus on clinicians acting as the central change agents driving adoption within their settings.
Underlying this approach is the importance of clinical audits with feedback, which are essential for assessing the impact of implemented changes and providing actionable insights.
Conclusion
The JBI's seven-phase process model provides a practical and systematic framework for healthcare professionals to effectively implement evidence into practice. By prioritizing collaboration, context analysis, facilitation, and continuous evaluation, this approach empowers clinicians to be active change agents, driving improvements in patient care and healthcare outcomes. However, ongoing research and development are crucial to further refine and validate the robustness of this approach, ensuring its adaptability to the complex and dynamic nature of evidence implementation.
Reference
Porritt K, McArthur A, Lockwood C, Munn Z. JBI's approach to evidence implementation: a 7-phase process model to support and guide getting evidence into practice. JBI Evid Implement. 2023 Mar 1;21(1):3-13. doi: 10.1097/XEB.0000000000000361. PMID: 36545902.
Review of Frameworks for Translating Research Evidence into Policy and Practice
Background
An examination of different frameworks for research translation, comparing similarities and differences, and identifying strengths and weaknesses when applied in practice.
Framework
- RE-AIM Framework:
- Evaluates research translation based on Reach, Efficacy, Adoption, Implementation, and Maintenance.
- Used in chronic disease management and public health.
- Knowledge Translation Continuum ('T' Models):
- Describes multiple phases from basic research (T0) to population health impact (T4).
- Originated in medical research but later adapted to public health.
- Knowledge to Action (KTA) Framework:
- Integrates knowledge creation (knowledge inquiry, synthesis, and tools) with an action cycle (implementation and evaluation).
- Focuses on tailoring knowledge to local contexts.
- PARiHS (Promoting Action on Research Implementation in Health Services) Framework:
- Emphasizes the interplay of Evidence, Context, and Facilitation in research implementation.
- Used in health services, particularly nursing and clinical practice.
- Evidence-Based Public Health (EBPH) Models:
- Focus on community assessment, evidence synthesis, and policy development.
- Applied in public health decision-making.
- Stages of Research and Evaluation Model ('Rocket Model'):
- Outlines steps from problem definition to intervention dissemination.
- Used in health promotion and chronic disease prevention.
- Interactive Systems Framework (ISF):
- Highlights the roles of prevention delivery, support, and translation in bridging research and practice.
- Applied in public health programs.
- UK Medical Research Council (MRC) Framework:
- A cyclical process of development, feasibility testing, evaluation, and implementation.
- Used in intervention research.
Key insights and implementation considerations
Implementing research translation frameworks is about providing a structured and systematic method to improve the adoption of evidence-based strategies in various health-related fields.
- Contextual Adaptation:
- Local Relevance: Tailor research evidence to fit the sociocultural, economic, and political context of the target population.
- Stakeholder Engagement: Involve policymakers, healthcare providers, and community members early in the process to increase acceptance and feasibility.
- Regulatory and Policy Alignment: Ensure the proposed intervention aligns with existing health policies, regulations, and institutional priorities.
- Capacity Building and Facilitation:
- Training and Education: Provide continuous training for healthcare professionals and decision-makers on how to apply research findings effectively.
- Organizational Readiness: Assess institutional capacity to implement and sustain the intervention, considering financial, technical, and human resources.
- Facilitation Mechanisms: Use knowledge brokers, champions, or facilitators to drive the adoption of evidence-based practices within healthcare settings.
- Research-to-Practice Translation Strategies:
- Simplified Knowledge Tools: Convert complex research findings into user-friendly formats such as guidelines, policy briefs, and decision-support tools.
- Pilot Testing: Conduct small-scale trials before full implementation to refine the intervention and address potential barriers.
- Iterative Feedback Mechanisms: Establish continuous monitoring and feedback loops to adapt strategies based on real-world experiences.
- Implementation and Scaling-Up Approaches:
- Multi-Sectoral Collaboration: Foster partnerships between academia, government, NGOs, and industry to enhance implementation success.
- Gradual Scaling: Implement interventions in phases, starting with high-priority areas before expanding nationwide.
- Resource Allocation: Ensure sustainable funding and logistical support for long-term program viability.
- Monitoring, Evaluation, and Sustainability:
- Evaluation Frameworks: Use models like RE-AIM to assess reach, effectiveness, adoption, implementation fidelity, and long-term sustainability.
- Data-Driven Decision Making: Leverage health information systems to track progress and inform policy adjustments.
- Sustainability Planning: Integrate interventions into existing healthcare structures to ensure long-term adoption beyond initial funding cycles.
Conclusion
The article concludes that conceptual models for research translation are interpreted and applied differently across diverse health fields. The reviewed models articulate processes for applying evidence from research to intervention development and subsequent dissemination into policy and practice. A common language is needed to help move the field forward in a coherent way and to describe better the processes and types of research associated with translating research evidence.
The implementation of knowledge translation frameworks into policy remains a complex but essential process for bridging the gap between research and practice. The review of eight research articles highlights key challenges, facilitators, and best practices in applying these frameworks effectively.
The frameworks reviewed share a common goal: improving the translation of research into policy by addressing barriers at different levels—individual, organizational, and systemic.
The successful translation of research into policy requires a multi-faceted, adaptive approach that considers political, institutional, and economic factors. By refining implementation strategies—through stakeholder collaboration, resource investment, and real-world evaluation—KT frameworks can play a pivotal role in shaping evidence-informed policies that improve population health outcomes.
Reference
Milat AJ, Li B. Narrative review of frameworks for translating research evidence into policy and practice. Public Health Res Pract. 2017;27(1):e2711704. https://dx.doi.org/10.17061/phrp2711704.