This section brings together a set of key frameworks and tools that are relevant to all phases of research into policy.
One Health Research Translation Framework →
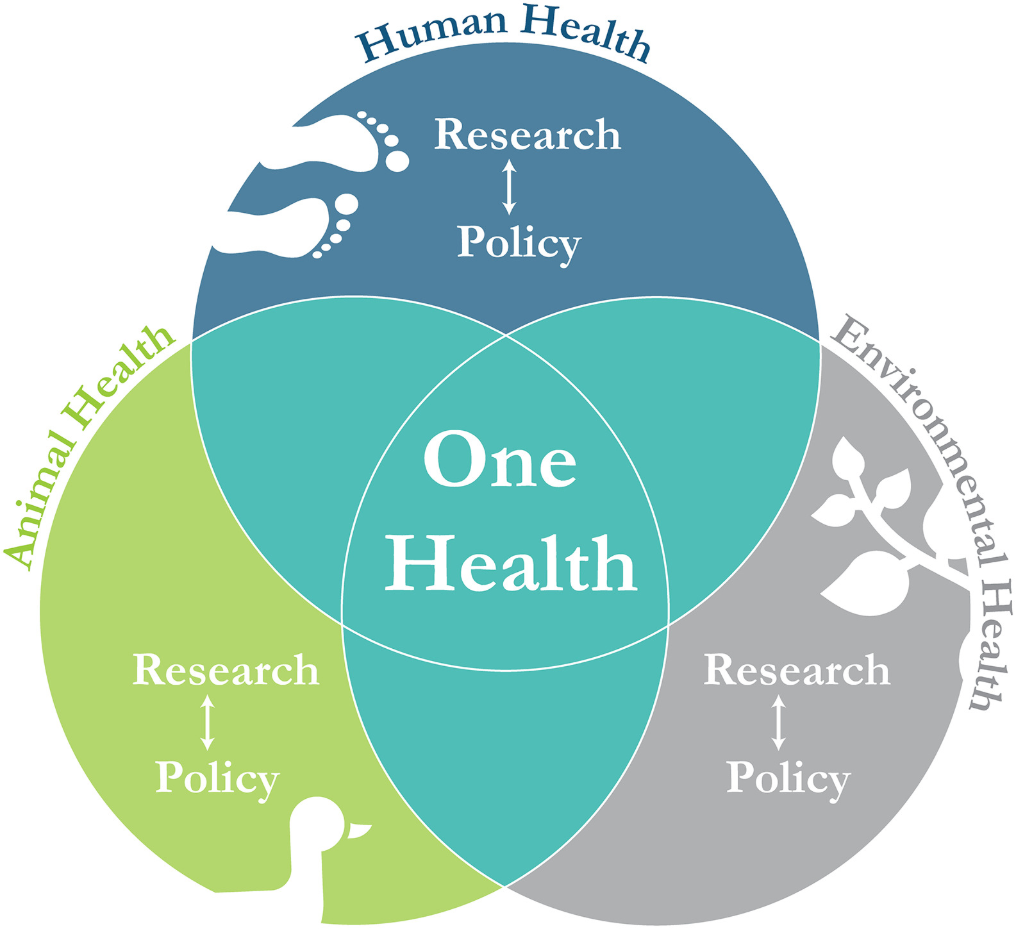
The One Health approach emphasizes the interconnectedness of human, animal, and environmental health, requiring cross-sector collaboration to effectively address health threats at their interface. Within this context, research translation plays a critical role in ensuring that scientific evidence informs the development of evidence-based policies and programs for the prevention and control of infectious diseases and other emerging threats.
Lost in Knowledge Translation →
This article addresses the challenge of translating research findings into real-world healthcare practice. It highlights the confusion surrounding terms like knowledge translation, transfer, and exchange, and proposes a conceptual framework to clarify the process of moving knowledge into action.
Contextualized Health Research Synthesis Program (CHRSP) →
The program provides timely, relevant, and easy-to-understand scientific evidence; optimizes evidence uptake; and, most importantly, attunes research questions and evidence to the specific context in which knowledge users must apply the findings. CHRSP was established with the goal of increasing the use of health evidence by decision makers.
Evidence-informed Decision Making in Public Health →
This article examines the role of values in health policy-making. It argues that while values are central to discussions about health systems and their reform, the concept of "value" itself remains vague, and policy-making processes often neglect values. The study aims to provide a model for value-based policy-making to clarify the concept of value and how it affects policy decisions.
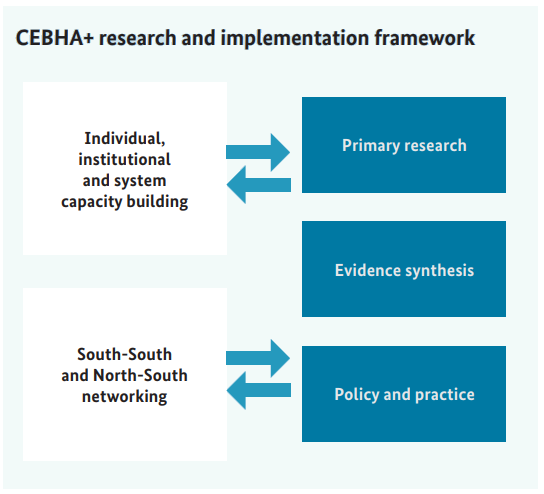
CEBHA + IKT: Evidence-based Healthcare and Public Health in Africa →
The long term goal of the network is to set up a long term capacity and infrastructure for evidence based healthcare and public health in sub Saharan Africa. The consortium seeks to strengthen African research institutions and promote competence in understanding and fast uptake of evidence in health system institutions.
Translation Science to Population Impact (TSci Impact) Framework →
This framework addresses two core challenges to the advancement of T2 translation research: (1) building infrastructure and capacity to support systems-oriented scaling up of evidence-based interventions, with well-integrated practice-oriented T2 research, and (2) developing an agenda and improving research methods for advancing T2 translation science.
One Health Research Translation Framework
Background
The One Health approach emphasizes the interconnectedness of human, animal, and environmental health, requiring cross-sector collaboration to effectively address health threats at their interface. Within this context, research translation plays a critical role in ensuring that scientific evidence informs the development of evidence-based policies and programs for the prevention and control of infectious diseases and other emerging threats.
To build effective national preparedness and response strategies, research translation must be a core component of capacity-building plans. However, there remains a need for conceptual guidance, training resources, and practical tools to support research translation efforts within a One Health framework.
The proposed One Health and research translation model simultaneously addresses integration gaps by connecting one health and research translation. It's a cyclical model that begins with research and continuously loops back, incorporating policy outcomes and emerging needs for ongoing refinement. It customises research applications to align with the unique cultural, systemic, and practical contexts of the target jurisdictions.
It facilitates effective communication and information sharing between researchers and policymakers to foster cross sector collaboration and mutual understanding. The model builds and strengthens the capabilities of individuals and organizations involved in research and policy to ensure sustainable, effective outcomes. The framework can be scaled and adapted to different contexts and settings while maintaining its core principles and effectiveness.
Conclusion
The One Health Research Translation Framework provides a structured, iterative process for integrating research into policy and practice to address zoonotic disease challenges. By supporting collaboration among research and policy stakeholders, the framework enhances the ability of health systems to respond to One Health threats with evidence-informed, context-specific interventions.
The Framework model
Reference
Casey Basham, Emily Billings, Amira S. El Rifay, Rebecca Badra, Mohamed A. Ali, Ali Asy, Samir Refaey, Ghazi Kayali, Corey Meyer, Designing and validating a One Health Research Translation Framework through literature-based case studies in Egypt, One Health,Volume 15,2022,100454,ISSN 2352-7714. https://doi.org/10.1016/j.onehlt.2022.100454 (https://www.sciencedirect.com/science/article/pii/S2352771422000866)
Lost in Knowledge Translation
Background
This article addresses the challenge of translating research findings into real-world healthcare practice. It highlights the confusion surrounding terms like knowledge translation, transfer, and exchange, and proposes a conceptual framework to clarify the process of moving knowledge into action.
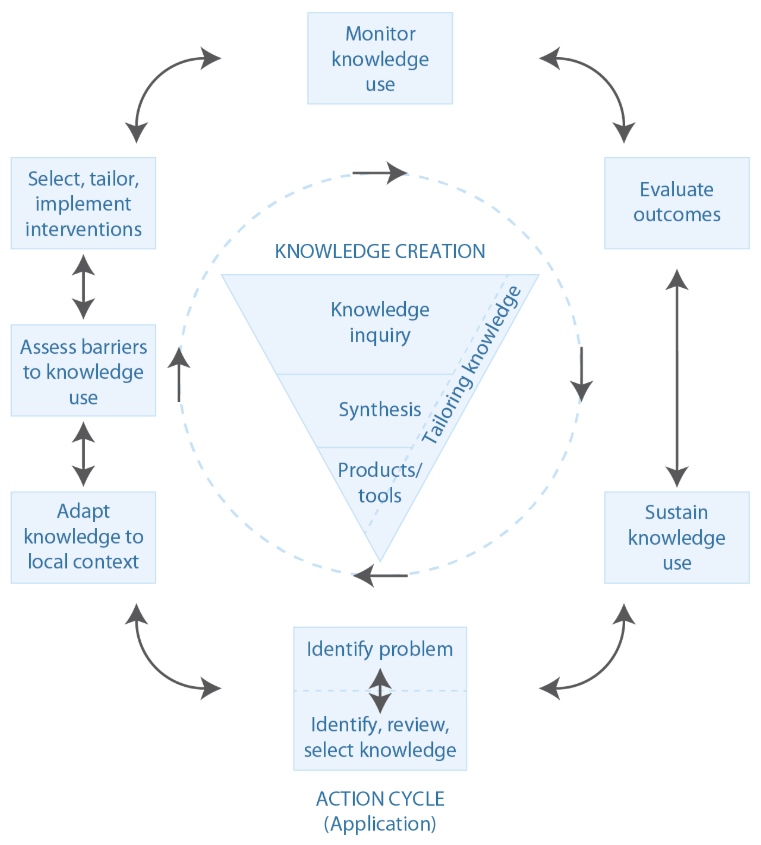
The Knowledge-to-Action (KTA) Framework
The KTA framework consists of two interconnected cycles:
- Knowledge Creation (The Knowledge Funnel)
- Knowledge Inquiry: The broad body of primary research.
- Knowledge Synthesis: Systematic reviews and meta-analyses that aggregate and evaluate evidence.
- Knowledge Products & Tools: Guidelines, decision aids, and frameworks designed to make evidence more accessible and actionable.
- Action Cycle (Application of Knowledge to Practice & Policy)
- Identifying a Problem: Determining an issue that requires an evidence-based solution.
- Adapting Knowledge to the Local Context: Ensuring that evidence is relevant to the specific setting.
- Assessing Barriers to Knowledge Use: Identifying obstacles in the implementation process.
- Selecting & Implementing Strategies: Choosing appropriate interventions for knowledge uptake.
- Monitoring Knowledge Use: Evaluating the application of research in practice.
- Evaluating Outcomes: Assessing the effectiveness of the implemented change.
- Sustaining Knowledge Use: Ensuring long-term integration of research findings into practice.
Key insights and implementation considerations
To begin, we have to define our target and what "moving knowledge into action" means. Too often researchers focus on making reports and academic papers. However, there are a plethora of alternative options that facilitate KTA: synopses in ACP Journal Club, care guidelines, decision aids, care pathways, creating better awareness and training for policymakers. This is the start of the planned-action theories and frameworks to help influence change in practice settings. The model suggests that to be effective in the real world, these interventions must be carefully tailored to fit local settings and circumstances. At all levels of planning, the user should consider such important steps as: establishing organizational buy-in, finding support from sources such as marketing, training, and technical assistance. The goal is to create a model to identify the relevant stakeholders and to establish a common understanding of KTA.
Conclusion
The authors conclude that because of a lack of consensus on what moving scientific research into policy is, a variety of processes and stakeholders must be included. In addition, there should be a clear articulation of responsibilities at all levels, as well as support and training from outside experts. The goal is a cycle of improvement that will be repeated and improved by the user.
Reference
Graham, Ian D. PhD1; Logan, Jo RN, PhD2; Harrison, Margaret B. RN, PhD3; Straus, Sharon E. MD, MSc4; Tetroe, Jacqueline MA5; Caswell, Wenda RN, MEd2; Robinson, Nicole6. Lost in knowledge translation: Time for a map?. Journal of Continuing Education in the Health Professions 26(1):p 13-24, Winter 2006. | DOI: 10.1002/chp.47 https://journals.lww.com/jcehp/abstract/2006/26010/lost_in_knowledge_translation__time_for_a_map_.3.aspx
Contextualized Health Research Synthesis Program (CHRSP)
Background
The program provides timely, relevant, and easy-to-understand scientific evidence; optimizes evidence uptake; and, most importantly, attunes research questions and evidence to the specific context in which knowledge users must apply the findings. CHRSP was established with the goal of increasing the use of health evidence by decision makers.
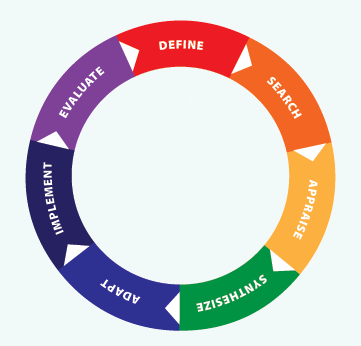
As an integrated knowledge translation (KT) method, CHRSP:
- Involves intensive partnerships with senior healthcare decision makers who propose priority research topics and participate on research teams;
- Considers local context both in framing the research question and in reporting the findings;
- Makes economical use of resources by utilizing a limited number of staff;
- Uses a combination of external and local experts; and
- Works quickly by synthesizing high-level systematic review evidence rather than primary studies.
By asking the health system to identify its own priorities and to participate directly in the research process, CHRSP fully integrates KT among researchers and knowledge users in healthcare. CHRSP synthesizes high-level evidence (systematic reviews and health technology assessments), produces reports quickly, and, most importantly, optimizes the relevance of its products to the concerns and capacities of decision makers by building an ongoing partnership with high-level provincial health-system leaders, having them generate the research questions and, above all, tailoring the presentation of findings to a carefully developed understanding of the context(s) in which these decision makers must operate.
Conclusion
A key objective of CHRSP is to maximize the use of limited, locally available resources and expertise to synthesize existing systematic reviews on topics chosen by local knowledge users and to interpret the findings considering local contextual factors.
Reference
Bornstein, S., Baker, R., Navarro, P. et al. Putting research in place: an innovative approach to providing contextualized evidence synthesis for decision makers. Syst Rev 6, 218 (2017). https://doi.org/10.1186/s13643-017-0606-4
Evidence-informed Decision Making in Public Health
Background
The process of distilling and disseminating the best available evidence from research, context and experience, and using that evidence to inform and improve public health practice and policy. Evidence-Informed Public Health (EIPH), the process of using the best available evidence from research, context, and experience in practice, can help adapting to changes to public health practice.
Evidence-informed decision making involves integrating the best available research evidence into the decision-making process. Additional factors—community health issues and local context, community and political preferences and actions, and public health resources—also play an important role. These four domains are represented by the coloured ovals at the right and may exert influence on decisions.
Understanding Research Evidence video series: 11 short and easy to understand videos that explain common concepts that you are likely to come across when exploring research.
The Framework
Conclusion
The model for Evidence-Informed Decision Making in Public Health is dynamic and in any given public health situation, the different factors may be weighed differently in making a final decision.
Reference
NCCMT 2025 Your Journey to Evidence-informed Decision Making in Public Health National Collaborating Centre for Methods and Tools
CEBHA+ IKT: Evidence-based Healthcare and Public Health in Africa
Background
The long term goal of the network is to set up a long term capacity and infrastructure for evidence based healthcare and public health in sub Saharan Africa. The consortium seeks to strengthen African research institutions and promote competence in understanding and fast uptake of evidence in health system institutions.
This network intends to translate the principles of evidence based public health by ensuring that the priority research questions are relevant and fill a real gap, through conducting robust research and through overcoming the disconnect between primary research, evidence synthesis and implementation into policy-and-practice.
Integrated knowledge translation (IKT) aims to establish mutually beneficial partnerships between researchers and decision-makers to increase the relevance and use of research for decision-making.
IKT processes and outcomes are evaluated using a comparative case study design. This yields a more refined programme theory of IKT that builds on effective and sustainable partnerships facilitating the translation of research into policy and practice.
The Framework
Reference
Collaboration for Evidence-Based Healthcare and Public Health in Africa(CEBHA+). Available at: Collaboration for Evidence-Based Healthcare and Public Health in Africa | Cochrane South Africa
Translation Science to Population Impact (TSci Impact) Framework
Background
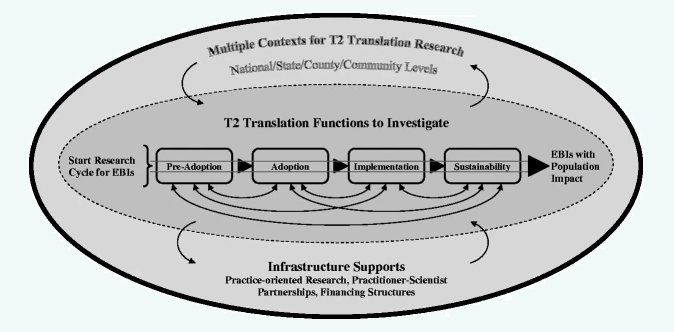
This framework addresses two core challenges to the advancement of T2 translation research:
(1) building infrastructure and capacity to support systems-oriented scaling up of evidence-based interventions, with well-integrated practice-oriented T2 research, and
(2) developing an agenda and improving research methods for advancing T2 translation science.
It articulates key considerations in addressing the core challenges, with three components that represent:
(1) four phases of translation functions to be investigated (pre-adoption, adoption, implementation, and sustainability);
(2) the multiple contexts in which translation occurs, ranging from community to national levels; and
(3) necessary practice and research infrastructure support.
There are two primary challenges limiting translation of evidence-based interventions (EBIs) into practice and the related gaps in Type 2 (T2) translational research, along with the consequences of these limits and gaps.
The two key proposed solutions include:
(1) building the necessary infrastructure and capacity to support the systems-oriented scale-up of EBIs and advanced practice-focused translational research, and
(2) developing a clearly defined research agenda and improved methodologies to address this agenda, to advance translation science.
In addition to these proposed solutions, specific strategies are needed to address the core challenges. These include synthesizing insights from prior studies and identifying future research priorities to close the evidence-to-practice gap. Finally, the role of government is critical—supportive policy changes, coordinated interagency efforts, and innovative, partnership-driven funding models are essential to foster both infrastructure development and scientific advancement in the field of translation research.
The Framework
Reference
Spoth, R., Rohrbach, L.A., Greenberg, M. et al. Addressing Core Challenges for the Next Generation of Type 2 Translation Research and Systems: The Translation Science to Population Impact (TSci Impact) Framework. Prev Sci 14, 319–351 (2013). https://doi.org/10.1007/s11121-012-0362-6